Find the perfect solution for your eye health needs

Protect Your Eyes This Holiday Season: The Impo...
Enjoy the summer holidays safely! Learn why UV protection for your eyes is essential and discover tips to keep your vision healthy this festive season.
Protect Your Eyes This Holiday Season: The Impo...
Enjoy the summer holidays safely! Learn why UV protection for your eyes is essential and discover tips to keep your vision healthy this festive season.
Christmas Gift Ideas from Eye Solutions: Perfec...
The holiday season is upon us, and it’s time to start thinking about the perfect gifts for your loved ones! If you’re looking for something thoughtful, stylish, and practical, Eye...
Christmas Gift Ideas from Eye Solutions: Perfec...
The holiday season is upon us, and it’s time to start thinking about the perfect gifts for your loved ones! If you’re looking for something thoughtful, stylish, and practical, Eye...

Discover Relief and Comfort: The Benefits of Ey...
Living with conditions like MGD (blepharitis), dry eye disease, chalazion (eyelid cysts), and other related eye issues can be challenging, affecting daily comfort and vision clarity. Heat compress masks, like The...
Discover Relief and Comfort: The Benefits of Ey...
Living with conditions like MGD (blepharitis), dry eye disease, chalazion (eyelid cysts), and other related eye issues can be challenging, affecting daily comfort and vision clarity. Heat compress masks, like The...
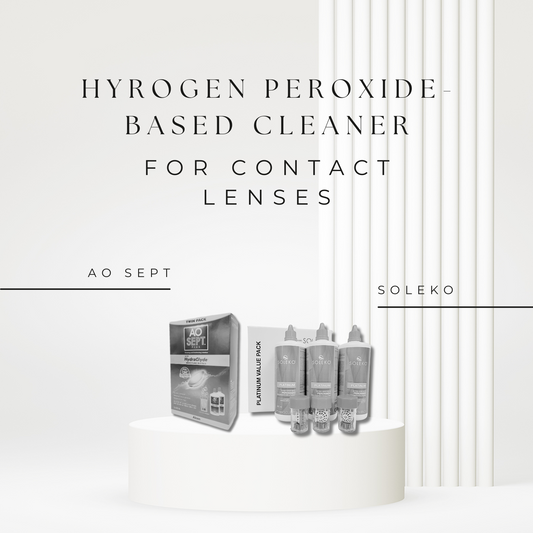
The Ultimate Guide to Using Hydrogen Peroxide-B...
Hydrogen peroxide cleaners are a game-changer in the world of contact lens care, offering a thorough and effective way to keep your lenses clean and your eyes healthy.
The Ultimate Guide to Using Hydrogen Peroxide-B...
Hydrogen peroxide cleaners are a game-changer in the world of contact lens care, offering a thorough and effective way to keep your lenses clean and your eyes healthy.

Embrace Comfort and Beauty: Mascara Safe for Se...
Eyes are not just windows to the soul; they tell stories of our emotions, experiences, and personality. Enhancing these expressive features can be as simple as finding the perfect mascara....
Embrace Comfort and Beauty: Mascara Safe for Se...
Eyes are not just windows to the soul; they tell stories of our emotions, experiences, and personality. Enhancing these expressive features can be as simple as finding the perfect mascara....

The Buzz About Manuka Honey: Benefits for Your ...
In the realm of eye care innovations, Optimel Eye Drops stand out as a remarkable fusion of science and nature, specifically crafted to address a range of eye health concerns....
The Buzz About Manuka Honey: Benefits for Your ...
In the realm of eye care innovations, Optimel Eye Drops stand out as a remarkable fusion of science and nature, specifically crafted to address a range of eye health concerns....
